A gene therapy for a rare type of severe combined immunodeficiency (SCID) was safe and sufficiently restored T-cell immunity in an early trial, results from a phase I/II study showed.
At a single center, all 10 infants with Artemis-deficient SCID (ART-SCID) produced functioning T cells at a median of 12 weeks after the procedure, reported Morton Cowan, MD, of UCSF Benioff Children’s Hospital in San Francisco, and colleagues.
Five of the six patients who were followed for at least 24 months had complete T-cell immune reconstitution at a median of 12 months, they noted in the New England Journal of Medicineopens in a new tab or window.
“I’ve transplanted [with bone marrow transplant] over 30 patients with Artemis deficiency, and it’s night and day,” Cowan told MedPage Today. “We’re seeing really good T-cell reconstitution, which we don’t see in a lot of the kids who get regular bone marrow transplants.”
Sung-Yun Pai, MD, a senior investigator at the National Cancer Institute, who wrote an accompanying editorialopens in a new tab or window, told MedPage Today that the evidence for T-cell reconstitution in the paper is “very, very strong.
“With a single treatment, nine out of 10 achieved T-cell counts that rescued them from opportunistic infection, which is the goal, and the 10th patient … had improvement in T-cell reconstitution with a second infusion,” Pai added.
SCID is genetically heterogeneous, caused by a defect in any one of about 20 genes, and it occurs in about one in 65,000 births in the U.S. ART-SCID is a rare form of the disease, accounting for only about 3% of all SCID cases, and it has a high incidence among people of Navajo or Apache descent and in some consanguineous populations.
Patients with ART-SCID generally have a poor response to standard treatment with allogeneic hematopoietic cell transplantation, even from a human leukocyte antigen (HLA)-matched donor, so researchers have been looking for alternative treatments.
Two other types of SCID — X-linked SCIDopens in a new tab or window (X-SCID) and adenosine deaminase deficiency SCIDopens in a new tab or window (ADA-SCID) — also have gene therapies in human trials, and gene therapies for other types of SCID are in preclinical trials, Cowan said.
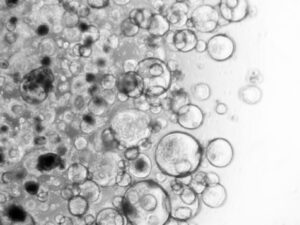
Cowan and colleagues used a novel lentiviral vector to transfect patients’ own CD34+ hematopoietic stem cells with a copy of the DCLRE1C gene, which encodes the Artemis protein. Cowan said lentiviral vectors have become a preferred vehicle since cases of leukemia were seen with earlier versions of gene therapy in SCID using other vectors. Lentiviral vectors have a lower risk of causing leukemia, he noted.
The new method also included a human promoter sequence to avoid toxic overexpression of the Artemis protein, while still delivering sufficient therapeutic levels. Earlier gene therapies have relied on viral promoters, Pai said, which could also play a role in increased cancer risk. Promoters control gene transcription and expression.
Another novel part of their approach was minimizing the dose of chemotherapy, using about 25% of the standard exposure to busulfan, since children with ART-SCID have an increased sensitivity to chemotherapy. Part of the rationale for lower-dose chemotherapy, Cowan said, was that sometimes children who receive full-dose chemotherapy before bone marrow transplant don’t develop permanent teeth, or develop dysfunctional ones, because those stem cells are wiped out.
The 10 infants were treated at UCSF Benioff from June 2018 to September 2021. None of them had an HLA-matched sibling for a bone marrow transplant.
Their median age at infusion was 2.7 months, and they were followed for a median of 31.2 months. Four patients were of Navajo or Apache descent and homozygous for the founder DCLRE1C mutation.
Researchers removed the babies’ hematopoietic stem cells, transfected them with the lentiviral vector containing the gene, and then re-infused the new cells a day after their second dose of busulfan.
All 10 children — some of whom have now been followed for 4 years — are healthy and all have adequate T-cell immunity, Cowan said.
Of the six children who were followed for at least 2 years, the only one who didn’t achieve full T-cell reconstitution had a cytomegalovirus (CMV) infection.
“He did get some T-cell immunity, but it wasn’t good enough to control this virus,” Cowan said. “We treated him again [with the gene therapy] and he’s doing quite well now. He’s gotten rid of the CMV, he’s living at home, and he’s gotten B cells. We’re hopeful that he’s going to be able to come off immune globulin in the spring.”
Indeed, all 10 children made B cells at a median of 6 weeks, which allowed for the discontinuation of immune globulin in four of the six children who were followed for at least 2 years.
Three of those patients had normal responses to childhood immunizations and formed protective antibodies, and since the data cutoff of June reported in the paper, a fourth child was able to get her shots and “has now responded beautifully to all her vaccinations,” Cowan noted.
Adverse events were as expected, the researchers said. Of the 17 grade 3 or 4 adverse events, 16 were cytopenias, likely due to bone marrow harvest or busulfan, they wrote.
Four patients developed autoimmune hemolytic anemia (AIHA), and Cowan added that a fifth patient has since developed AIHA.
“It does seem to disappear after they’ve reconstituted their T-cell immunity,” he noted.
Of those five children, one was hospitalized for a blood transfusion but is now fine, off medications, and living a normal life, Cowan said. One child’s AIHA was only detected via monitoring and never required therapy, and the other three only needed outpatient treatment, he added.
Still, the authors noted that additional follow-up with a larger sample will be necessary to characterize AIHA in this patient population.
Cowan said that there was no evidence of clonal expansion or cancer, but that these patients will need to be followed closely to make sure that no cancer develops.
Pai said she has fewer concerns about cancer with this approach because the promoter is derived from the human Artemis gene itself and shouldn’t be as potent in terms of expression compared with a viral promoter.
However, lentiviral vector therapy has been associated with the development of canceropens in a new tab or window in a gene therapy for adrenoleukodystrophy made by Bluebird Bio. One patient developed myelodysplastic syndrome (MDS) about a year after treatment, and two others had bone marrow abnormalities that could lead to MDS.
But that therapy used a viral promoter, not a human promoter, to drive gene expression, Pai said.
The ART-SCID gene therapy also lacks an insulator that was used in a gene therapy trial in X-SCID that may be problematic, in that it led to the development of abnormal proteins. “It makes you a little worried that if it keeps growing out of control, it will become cancer,” she said.
“Only time can tell whether the vector will ultimately be safe in the long term,” she added.
Nonetheless, Pai said, the ART-SCID gene therapy is an important advance over the standard of care of bone marrow transplant because it “avoids the problems that come with using donor cells, and it obviates the need to find a well-matched donor. There are plenty of people who don’t have matched donors available to them.”
She added that she was particularly glad to see how well the therapy was working for the Navajo and Apache populations “who may not always have access even to standard therapy.”
As for next steps, Cowan said his group is working with the FDA with the aim of starting their pivotal trial next year. In the meantime, they are continuing their phase I/II study and have just enrolled their 11th patient.
Original article posted in MedPage Today.